by Matt Mazewski, Ph.D. 1
1 Myodesopsia International
Cite as: Mazewski, M. (2023). Hypothesis: Symptomatic myodesopsia/vitreous floaters may constitute a risk factor for Long COVID and ME/CFS. Patient-Generated Hypotheses Journal for Long COVID & Associated Conditions, Vol. 1, 13-20
Abstract
The ophthalmological condition known as myodesopsia or vitreous floaters results from aggregates of proteins or cellular debris in the vitreous body casting shadows onto the retina that are perceived as objects moving through the visual field. While this is commonly viewed as a benign condition associated with aging, a growing body of research suggests that for some patients it can severely impact visual function and quality of life. Myodesopsia is often caused by posterior vitreous detachment, but can also result from other conditions such as asteroid hyalosis, uveitis, or myopic vitreopathy. There are strong reasons to suspect that its presence may be indicative of a susceptibility to collagen degradation in response to inflammatory triggers, which may represent a risk factor for the development of Long COVID, ME/CFS, or related chronic illnesses. Evidence for such susceptibility includes the presence of collagen-degrading enzymes in the vitreous, associations with other connective tissue disorders, and links between myodesopsia and infections with various pathogens.
Introduction
Myodesopsia, also known as vitreous floaters or “eye floaters,” is an ophthalmological condition in which aggregations of proteins or other cellular debris within the vitreous body, the normally transparent gel that occupies the space between the retina and lens, cast shadows onto the retina that are perceived as objects moving through the visual field1. Clinicians have traditionally viewed myodesopsia as a common and mostly benign phenomenon associated with normal aging that only causes significant disability or morbidity very rarely, if at all2. A growing body of research has shown, however, that for a subset of patients the impact on visual function and quality of life can be severe3,4,5,6.
In older adults, the leading cause of myodesopsia is an age-related development known as posterior vitreous detachment (PVD), which occurs when the vitreous undergoes collapse and detaches from the retina due to progressive liquefaction of its gel structure. Symptomatic floaters are often found in younger individuals as well though, even if their exact prevalence has not been established. In patients without PVD, floaters may result from conditions such as asteroid hyalosis, uveitis, or, more commonly, myopic vitreopathy7.
Although the precise etiological mechanisms behind myodesopsia in many instances remain unknown – and the condition is often therefore deemed “idiopathic”—there are strong reasons to suspect that such cases may be indicative of a susceptibility to collagen degradation in response to inflammatory triggers. This in turn may represent a risk factor for the development of Long COVID, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), or related chronic illnesses. There is evidence that collagen breakdown may be a significant factor in these diseases insofar as it is a correlate of damage to structurally important connective tissues, such as the ligaments of the craniocervical junction8.
Hypothesis
We review here three reasons why floaters may be a sign of vulnerability to such breakdown.
First, collagen-degrading enzymes are present in human vitreous and are likely involved in structural changes thereto. The vitreous is an extracellular matrix (ECM) that consists of roughly 98% water and 2% structural macromolecules, chief among them hyaluronan and collagen (including types II, IX, and a hybrid of types V and XI)7. It also contains varying concentrations of matrix metalloproteinases (MMPs), proteolytic enzymes that are believed to play a role in age-related vitreous liquefaction9. These include MMP-1 (interstitial collagenase), MMP-2 (gelatinase A), MMP-3 (stromelysin-1), and MMP-9 (gelatinase B)10. Indeed, pharmacological inhibitors of MMP activity have been proposed as candidates for prophylaxis of vision-degrading myodesopsia7. An implication is that symptomatic floaters in younger patients could be evidence of a greater-than-ordinary propensity to MMP upregulation and collagen breakdown, including in response to infection.
Second, myodesopsia has been identified as a comorbidity in other connective tissue disorders, some of which themselves potentially increase risk for the development of Long COVID and ME/CFS11. Sebag (2014) describes known associations with Marfan syndrome and Ehlers-Danlos syndrome (EDS)12. Milhorat et al. (1999) note that “floaters or flashing lights” were reported by 200 out of 364 patients (54.9%) with a diagnosis of Chiari I malformation or syringomyelia13. (To put this figure in context, one 2021 survey of ophthalmologists and optometrists found that “only” between 17% and 32% of all patients reporting to the typical clinic for an ocular examination have some amount of symptomatic floaters14.) In a 2013 lecture on cervical medullary syndrome, which involves structural compression of the brainstem, Dr. Roger Kula explicitly hypothesized that the high prevalence of floaters in this patient population was due to a correspondingly high predisposition for connective tissue disorders (see at 17:00 in the cited recording)15.
Third, there are known links between myodesopsia and infection with various pathogens, such as Borrelia16, Bartonella17, and Toxoplasma18, suggesting that the presence of floaters may be evidence of a prior collagen-degrading infectious process even when a specific causative agent cannot be identified. Floaters have already been highlighted in the literature as a possible ocular sequela of COVID-19 itself19, and online forums and support groups for myodesopsia sufferers are now filled with anecdotal reports of onset following SARS-CoV-2 infection or even COVID vaccination (see the appendix for a sampling of recent anonymized reports of floater onset following SARS-CoV-2 infection or vaccination from the Reddit communities r/CovidLongHaulers and r/EyeFloaters, which currently have over 45,000 and 6,000 members, respectively)20,21.
How to test the hypothesis
Testing this hypothesis would ideally entail conducting a well-powered prospective longitudinal study in which individuals with and without symptomatic myodesopsia would be followed for a period of time so that the incidence of Long COVID or ME/CFS in both groups could be ascertained. For study purposes, a diagnostic definition of myodesopsia should be adopted that incorporates both patients’ own symptom reports as well as objective clinical indicators like contrast sensitivity function and vitreous echodensity as measured by quantitative ultrasound22.If the hypothesis is correct, it would suggest that a relatively simple ocular screening might be a cost-effective way of identifying at least one subset of patients at higher risk for these serious conditions. It would also provide an additional rationale for performing genetic studies aimed at uncovering as yet unknown mutations associated with a tendency to developing them, which could in the future enable a more targeted approach to prevention of myodesopsia as well as of various complex chronic illnesses.
References
1 Sauvage, F., Nguyen, V. T., Li, Y., Harizaj, A., Sebag, J., Roels, D., Van Havere, V., Peynshaert, K., Xiong, R., Fraire, J. A., Tassignon, M., De Smedt, S. C., Paulus, Y. M., Braeckmans, K., & De Smedt, S. C. (2022). Laser-induced nanobubbles safely ablate vitreous opacities in vivo. Nature Nanotechnology, 17(5), 552–559. https://doi.org/10.1038/s41565-022-01086-4
2 European Society of Cataract and Refractive Surgeons (ESCRS).(2022). Vitrectomy for floaters? https://www.escrs.org/eurotimes-articles/vitrectomy-for-floaters
3 Sebag, J. (2011). Floaters and the quality of life. American Journal of Ophthalmology, 152(1), 3-4.e1. https://doi.org/10.1016/j.ajo.2011.02.015
4 Wagle, A. M., Lim, W., Yap, T., Neelam, K., & Eong, K. A. (2011). Utility values associated with vitreous floaters. American Journal of Ophthalmology, 152(1), 60-65.e1. https://doi.org/10.1016/j.ajo.2011.01.026
5 Zou, H., Liu, H., Xu, X., & Zhang, X. (2013). The impact of persistent visually disabling vitreous floaters on health status utility values. Quality of Life Research, 22(6), 1507–1514. https://doi.org/10.1007/s11136-012-0256-x
6 Milston, R., Madigan, M. C., & Sebag, J. (2016). Vitreous floaters: Etiology, diagnostics, and management. Survey of Ophthalmology, 61(2), 211–227. https://doi.org/10.1016/j.survophthal.2015.11.008
7 Sebag, J. (2020). Vitreous and vision degrading myodesopsia. Progress in Retinal and Eye Research, 79, 100847. https://doi.org/10.1016/j.preteyeres.2020.100847
8 Proal, A. D., & VanElzakker, M. B. (2021). Long COVID or post-acute sequelae of COVID-19 (PASC): An overview of biological factors that may contribute to persistent symptoms.. Frontiers in Microbiology, 12. https://doi.org/10.3389/fmicb.2021.698169
9 Vaughan-Thomas, A., Gilbert S. J., & Duance, V. C. (2000). Elevated levels of proteolytic enzymes in the aging human vitreous. Investigative Ophthalmology and Visual Science, 41(11), 3299-3304.
10 Plantner, J. J., Smine, A., & Quinn, T. J. (1998). Matrix metalloproteinases and metalloproteinase inhibitors in human interphotoreceptor matrix and vitreous. Current Eye Research, 17(2), 132–140. https://doi.org/10.1076/ceyr.17.2.132.5610
11 Eccles, J. A., Thompson, B. E., Themelis, K., Amato, M. C. M., Stocks, R., Pound, A., Jones, A., Cipinova, Z., Shah-Goodwin, L., Timeyin, J., Thompson, C., Batty, T., Harrison, N. A., Critchley, H. D., & Davies, K. M. (2021). Beyond bones: The relevance of variants of connective tissue (hypermobility) to fibromyalgia, ME/CFS and controversies surrounding diagnostic classification: An observational study. Clinical Medicine, 21(1), 53–58. https://doi.org/10.7861/clinmed.2020-0743
12 Sebag, J. (2014). Reassessing the surgical treatment of floaters. Retina Today, 1-4. https://www.vmrinstitute.com/wp-content/uploads/2015/06/Surgical-Treatment-of-Floaters-RETINA-TODAY-2014.pdf
13 Milhorat, T. H., Chou, M. W., Trinidad, E. M., Kula, R. W., Mandell, M., Wolpert, C. M., & Speer, M. C. (1999). Chiari I malformation redefined: Clinical and radiographic findings for 364 symptomatic patients. Neurosurgery, 44(5), 1005–1017. https://doi.org/10.1097/00006123-199905000-00042
14 D’Amico, D., Berrocal, M. H., Ho, A. C., Houston, S. K. S., Kitchens, J., Morris, R., Ryan, E. H., Silva, R. A., & Weng, C. Y. (2021). Survey findings on vitreous opacities and expert panel recommendations on the referral and management of symptomatic vitreous opacity cases. Retina Today. https://retinatoday.com/articles/2021-nov-dec-supplement4/survey-findings-on-vitreous-opacities-and-expert-panel-recommendations-on-the-referral-and-management-of-symptomatic-vitreous-opacity-cases
15 Bobby Jones Chiari & Syringomyelia Foundation. (2013, December 2). CSF presents clinical patterns seen with cervical medullary syndrome [Video]. YouTube. https://www.youtube.com/watch?v=p2cTNY7-LyA
16 Lindström, B., Skogman, B. H., Lindström, A. K., Tallstedt, L., & Nilsson, K. (2022). Borrelia ocular infection: A case report and a systematic review of published cases. Ophthalmic Research, 65(2), 121–130. https://doi.org/10.1159/000521307
17 Kiu, K., Hanizasurana, H., & Zunaina, E. (2015). Neuroretinitis with dual infections. International Medical Case Reports Journal, 8, 255-258. https://doi.org/10.2147/imcrj.s91323
18 Song, A. T. W., Scott, I. U., Davis, J. L., & Lam, B. L. (2002). Atypical anterior optic neuropathy caused by toxoplasmosis. American Journal of Ophthalmology, 133(1), 162–164. https://doi.org/10.1016/s0002-9394(01)01211-9
19 Kodati, S., McHarg, M., Wang, Y., Caplash, S., Yakin, M., & Sen, H. N. (2021). Ocular symptoms in COVID-19 infection: A survey study. Investigative Ophthalmology and Visual Science, 62(8), 1968. https://doi.org/10.1186/s12348-022-00319-w
20 r/CovidLongHaulers. (n.d.). Reddit. https://www.reddit.com/r/covidlonghaulers/
21 r/EyeFloaters. (n.d.). Reddit. https://www.reddit.com/r/EyeFloaters/
22 Mamou, J., Wa, C. A., Yee, K. M., Silverman, R. H., Ketterling, J. A., Sadun, A. A., & Sebag, J. (2015). Ultrasound-based quantification of vitreous floaters correlates with contrast sensitivity and quality of life. Investigative Ophthalmology & Visual Science, 56(3), 1611–1617. https://doi.org/10.1167/iovs.14-15414
Appendix: Anonymized anecdotal reports of myodesopsia onset following SARS-CoV-2 infection or COVID vaccination from online communities
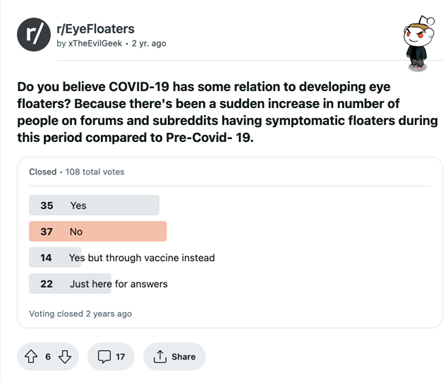
Figure 1. Poll from the Reddit community r/EyeFloaters on the relationship between COVID and developing eye floaters. Source: https://www.reddit.com/r/EyeFloaters/comments/qhtek3/do_you_believe_covid19_has_some_relation_to/
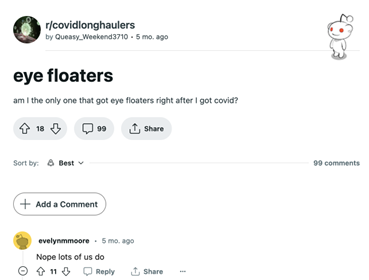
Figure 2.1, 2.2. Post from the Reddit community r/covidlonghaulers on eye floaters after COVID. Source: https://www.reddit.com/r/covidlonghaulers/comments/zt6nc4/eye_floaters/

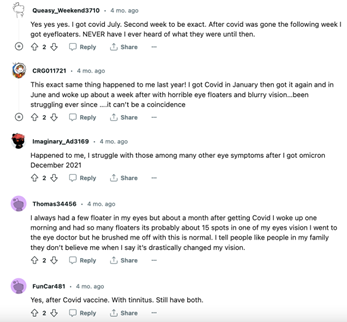
Figure 3.1, 3.2. Post from the Reddit community r/EyeFloaters on COVID Correlation. Source: https://www.reddit.com/r/EyeFloaters/comments/1068b8v/covid_correlation/

Figure 4. Post from the Reddit community r/EyeFloaters on floaters after COVID vaccine. Source: https://www.reddit.com/r/EyeFloaters/comments/pl013m/floaters_after_covid_vaccine/